Biosimilars represent a dynamic frontier in the biopharmaceutical sector, mirroring the complexities and promising potentials of their reference biologics—innovative biological medicines made from living cells. Unlike standard generics, biosimilars are not exact copies but are highly similar to an original product, with no clinically meaningful differences in terms of safety, purity, and potency.
What are Biosimilars
A biosimilar is officially defined as a biologic medical product that is highly similar to an already approved biological reference medicine. It matches the reference product in terms of structure, biological activity, and efficacy, ensuring no significant differences in safety and effectiveness. The minor differences in clinically inactive components are acceptable and do not alter the clinical outcome.
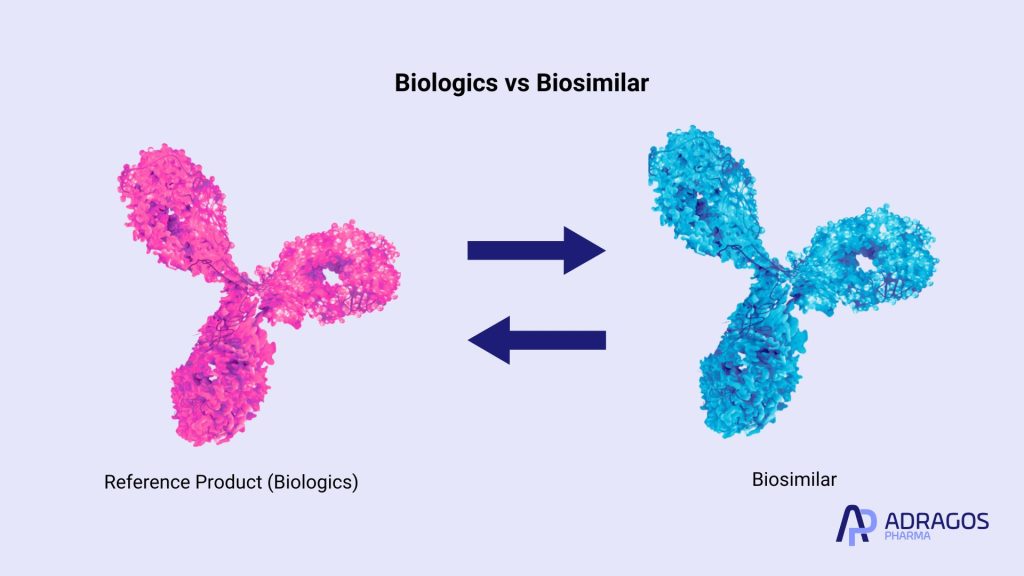
Biosimilars vs Biologics
While biosimilars and their reference biologicals share therapeutic goals, they differ fundamentally in their development and approval processes. Biologicals, or biologics, are original therapies derived from living organisms, complex in structure and function. In contrast, biosimilars are not exact copies but highly similar versions of these biological medicines. They require rigorous testing to demonstrate that there are no significant differences in safety, efficacy, and purity compared to the original biological reference medicine. This ensures that biosimilars provide a comparable therapeutic effect, making them a more accessible alternative due to potentially lower costs and similar clinical outcomes.
Biosimilars vs Generics
Generics are exact chemical replicas of small-molecule drugs, requiring proof of chemical equivalence for approval. They replicate the active ingredient, route, dosage, and performance of the original drug exactly. Conversely, biosimilars are not identical but must be highly similar to their biological medicines known as reference products. Due to the complex nature of biologics derived from living cells, biosimilars must undergo rigorous testing to show they have no clinically meaningful differences in safety and efficacy from their references. This process is more complex and regulated than for generics, emphasizing the quality and therapeutic equivalence needed for clinical use.
The Journey from Concept to Clinical Trials and Clinical Practice
Developing biosimilars is an intricate process that demands a deep understanding of the biological source and the manufacturing process used to create the original medicine. Biosimilar development requires stringent evaluation to ensure that each biosimilar can confidently be considered equivalent to the reference medicine it seeks to emulate.
The Role of Regulation in Biosimilar Approval: Ensuring Safety and Efficacy
Regulatory frameworks play a pivotal role in the biosimilar landscape. Understanding the approved indications is crucial, as it highlights which conditions biosimilars are approved for and ensures their appropriate use. Entities like the European Medicines Agency and the FDA set high standards for approval, ensuring safety and efficacy through comprehensive clinical trials and analytical studies. These bodies scrutinize everything from the scientific rationale behind each biosimilar to the detailed outcomes of clinical practice scenarios.
Biosimilars in the Market: Challenges and Opportunities
The path to market for biosimilars is fraught with both hurdles and opportunities. From navigating complex patent environments to addressing biosimilar medicines pricing pressures, developers must operate within a highly competitive space. The strategic incorporation of robust IP tactics and regulatory expertise is essential for achieving market success.
Economic Implications: Cost-Effectiveness and Patient Access
Biosimilars are poised to play a crucial role in healthcare economics by potentially lowering the costs associated with expensive biologic therapies. This cost-effectiveness helps broaden patient access to vital treatments, particularly for chronic conditions like rheumatoid arthritis and autoimmune diseases.
Clinical Applications and Global Impact
Globally, the adoption of biosimilars varies, influenced by regional regulatory guidelines and healthcare infrastructure. In many parts of the world, including the European Union, biosimilars have become a staple in treatment options, proving essential in areas like oncology and immunology.
Innovations and Future Trends in Biosimilar Development
The future of biosimilars lies in ongoing innovation and adaptation. Advances in biotechnological methods and a deeper understanding of biological medicines could lead to even more effective and accessible biosimilar products. The industry’s commitment to research and development is critical in shaping a future where biosimilars are a mainstream part of medical treatment.
Patient-Centric Approaches: Educating and Empowering Stakeholders
Education remains a cornerstone of biosimilar adoption. Healthcare professionals need to be well-informed about the benefits and considerations of prescribing biosimilars. Similarly, patient education is crucial to empower individuals in making informed decisions about their health and treatment options.
The Role of Biosimilars in Enhancing Healthcare Quality
The integration of biosimilars into clinical practice signifies a major leap forward in enhancing healthcare quality and efficacy. By providing equivalent therapeutic outcomes at potentially lower costs, biosimilars help ensure that more patients can receive the high-quality treatment they need.
Biosimilars represent a significant advancement in the pharmaceutical field, offering safe, effective, and more affordable alternatives to costly biologic therapies. Their continued development and integration into global healthcare systems promise to not only enhance patient outcomes but also drive innovation and competition in the biopharmaceutical industry.
FAQs about Biosimilars
What is a biosimilar with example?
An example of a biosimilar is Inflectra, a biosimilar to the immunosuppressive drug Remicade (infliximab). Both are used to treat conditions like rheumatoid arthritis and ulcerative colitis, ensuring the same therapeutic effect for patients.
What is a biosimilar vs. generic?
A generic drug is an exact copy of a chemical drug, while a biosimilar closely mimics a biologic drug which is typically derived from living organisms. Biosimilars are similar but not identical to their reference products due to the natural variability of biological expression in living cells.
What is a biosimilar NHS?
In the NHS (National Health Service in the UK), biosimilars are seen as a cost-effective alternative to more expensive biologics, helping to improve patient access to necessary high-quality treatments while managing healthcare expenditures.
Are biosimilars safer than biologics?
Biosimilars are as safe as their reference biologics. They undergo rigorous testing to ensure they meet high standards of safety, efficacy, and quality.
Is aspirin a biosimilar?
No, aspirin is not a biosimilar. It is a small-molecule drug, chemically synthesized and not based on a biologic.
Is insulin a biosimilar?
Insulin can be a biosimilar if it mimics a previously approved biologic insulin product. There are biosimilar versions of insulin intended to provide similar treatment outcomes at lower costs.
What is another name for biosimilars?
Biosimilars are also often referred to as follow-on biologics in some regions.
What are the advantages of biosimilar drugs?
The advantages of biosimilar drugs include reduced healthcare costs, increased access to treatment, and stimulating competitive pricing in the market, all while maintaining similar efficacy and safety profiles as their reference biologics.