Clinical trial material (CTM) is fundamental to the drug development process, acting as the bridge between laboratory research and the first evaluations of new drug products in human subjects. For pharmaceutical companies, understanding the essential components and best practices for manufacturing CTM is crucial to ensure patient safety, regulatory compliance, and reliable clinical trial outcomes. The following sections explore what clinical trial material is, how it is produced and controlled, and why meticulous planning and quality assurance are critical at every stage of clinical trials.
What is Clinical Trial Material (CTM) and Its Crucial Role
Clinical trial material (CTM) is at the very heart of clinical research and drug development. CTM includes all forms of the drug product—such as investigational medicinal products, investigational drugs, placebos, and comparators—specifically manufactured for use in clinical trials on human subjects. These materials are prepared to meet the highest standards of safety, quality, and efficacy, as specified by regulatory bodies like the FDA and European Medicines Agency. At this stage, the product leaves the laboratory as trial material and becomes the human-ready dose tested in real-world clinical studies. The quality and reliability of CTM are pivotal for safeguarding trial participants and for collecting data that accurately reflects the product’s therapeutic potential.
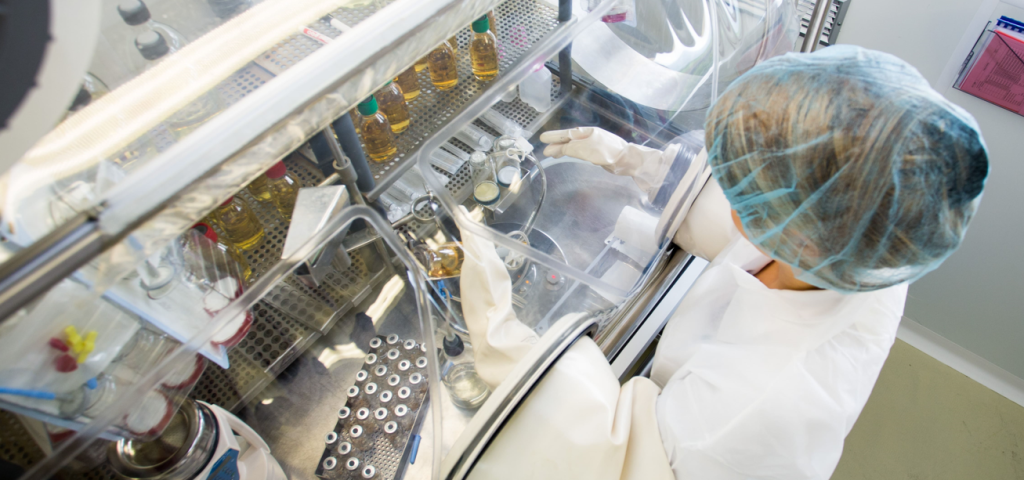
The Complex Process of Clinical Trial Material Manufacturing
The transition from small-scale laboratory work to clinical trial manufacturing involves implementing specific clinical manufacturing processes that introduce significant challenges. Unlike making small research batches, manufacturing clinical trial materials requires robust processes that adhere to cGMP guidelines and good manufacturing practices (GMP), and following GMP guidance. This involves the scale up and manufacture of clinical trial materials without sacrificing consistency, managing new sources of variability, and producing enough material for multiple trial sites or large-scale clinical trials. The manufacturing process must be validated to guarantee every dose has identical composition and quality, supported by detailed documentation and quality control steps. From qualifying the equipment—ensuring all equipment and materials are properly identified and documented—to training specialized personnel and adapting workflows, every element is designed to meet strict regulatory requirements and ensure patient safety.
Key Steps in Planning and Execution
A successful CTM project always begins with proactive planning. This planning involves building a realistic timeline that accounts not only for drug substance production but also for unavoidable losses (like overfill and destructive batch sampling) and the time needed for regulatory submissions. Before the clinical batch is filled, advanced analytical and stability testing must demonstrate the drug product’s robustness. Companies must identify and assemble a multidisciplinary team—including regulatory, process development, and clinical manufacturing experts—or partner with a specialized contract development and manufacturing organization (CDMO). During phase I and II development, it is especially important to ensure compliance with cGMP guidelines and robust quality control, as these early stages set the foundation for later success. This collaborative approach helps companies successfully navigate both operational and regulatory hurdles along the way.
The Pillars of Quality: Qualification, Validation, and Documentation
Ensuring the quality and consistency of CTM relies on meticulous attention to three interconnected components: qualification, validation, and documentation. Qualification involves detailed checks of equipment, selection of suitable containers and packaging, and training manufacturing teams. Validation tackles the proof that every clinical batch—regardless of size or complexity—can be produced identically, as required for trial material. This often means running test batches and validating each analytical process step. The final pillar, documentation, involves creating comprehensive manufacturing records. Regulators and quality assurance teams depend on this documentation to trace every action, rationale, and outcome during the CTM manufacturing process, which is essential for regulatory compliance during all clinical phases and for ensuring the traceability and quality of the final product—the completed, packaged, and ready-to-distribute drug formulation.
Formulations and Packaging: Addressing Unique Challenges in Clinical Trial Material
Every clinical trial material manufacturing campaign must address the unique challenges posed by specialized formulations and packaging requirements. Whether producing injectables, oral liquids, solid tablets, or cutting-edge gene therapy drugs, the goal is to ensure patient safety and ease of delivery throughout the duration of clinical trials. The choice of packaging—sometimes even individualized packaging for personalized medicine or adaptive trial designs—can be individual patients based, tailoring treatments and packaging to each patient’s unique genetic, environmental, and lifestyle needs. Regulatory authorities such as the FDA and European Medicines Agency impose strict guidelines on packaging as well as labeling, ensuring materials remain potent and traceable all the way to the individual patient or trial site.
Regulatory Requirements: Navigating Compliance in Clinical Trial Material
Regulatory requirements form the backbone of clinical trial material manufacturing, ensuring that every step of the process—from initial production to final distribution—meets the highest standards of quality and safety. Agencies such as the FDA and the European Medicines Agency (EMA) set strict guidelines for the manufacturing, packaging, labeling, and distribution of investigational medicinal products. Adhering to these good manufacturing practices (GMP) is not just a legal requirement; it is essential for protecting trial participants and maintaining the integrity of clinical research.
Successfully navigating compliance means understanding and implementing the latest regulatory requirements for clinical trial materials. This includes robust quality control procedures, meticulous record-keeping, and validated manufacturing processes that can withstand regulatory scrutiny. The FDA, for example, provides detailed guidance on GMP requirements for clinical trials, emphasizing the need for comprehensive documentation and consistent quality standards throughout the manufacturing process.
Regulatory agencies routinely conduct inspections to verify that manufacturers are following GMP guidelines and that clinical trial materials are suitable for human use. These inspections assess everything from the cleanliness of manufacturing facilities to the accuracy of packaging and labeling. Manufacturers must also be prepared to manage the unique challenges of clinical research, such as scaling up production for larger trials while ensuring supply chain integrity and product consistency.
As the landscape of clinical trials evolves, so too do regulatory requirements. Manufacturers must stay informed about new guidance and adapt their processes accordingly to ensure ongoing compliance. By prioritizing regulatory requirements and good manufacturing practices, organizations can confidently deliver high-quality clinical trial materials that meet the expectations of both regulators and trial participants.
The Role of CDMOs: Strategic Partnerships in Clinical Trial Supply
Contract Development and Manufacturing Organizations (CDMOs) have become indispensable partners in the clinical trial supply chain, offering specialized expertise and resources for manufacturing clinical trial materials. These organizations provide a comprehensive suite of services, including formulation development, manufacturing, packaging, labeling, and distribution, all tailored to the unique demands of clinical research.
Strategic partnerships with CDMOs enable sponsors to successfully navigate the complexities of clinical trial material manufacturing. CDMOs bring deep knowledge of GMP requirements, regulatory guidelines, and quality control procedures, ensuring that every batch of clinical trial materials meets the highest standards for safety and efficacy. Their experience in managing manufacturing processes and scaling up production is particularly valuable for sponsors preparing for larger scale clinical trials or introducing new treatments such as gene therapy and personalized medicine.
By leveraging the capabilities of a CDMO, sponsors can reduce the risk of delays, minimize supply chain disruptions, and ensure that clinical trial materials are manufactured and distributed in full compliance with regulatory requirements. CDMOs also offer flexible solutions for adaptive trial designs and targeted therapies, supporting the development of innovative treatments for individual patients.
Selecting the right CDMO is a critical decision for any clinical trial sponsor. A strong partnership can provide guidance on every aspect of the manufacturing process, from initial development to final distribution, helping sponsors to achieve their clinical and regulatory milestones efficiently and cost-effectively.
Benefits of Specialized Clinical Trial Manufacturing
Specialized clinical trial manufacturing delivers a host of advantages that can significantly enhance the success of clinical trials. By adopting advanced manufacturing processes—such as on-demand or bright-stock manufacturing—sponsors gain increased flexibility to respond to changing trial needs, reducing the risk of supply shortages or interruptions.
One of the key benefits of specialized manufacturing is the ability to support adaptive trial designs and targeted therapies, which are increasingly important in modern clinical research. These approaches allow for more personalized treatment of individual patients, improving both the patient experience and the overall effectiveness of clinical trials. Specialized manufacturing processes can also help minimize waste and optimize production, resulting in cost savings and greater efficiency.
Furthermore, specialized clinical trial manufacturing ensures that all materials are produced in accordance with GMP guidelines and regulatory requirements, maintaining the highest standards of quality and safety. This focus on quality control not only protects trial participants but also supports the generation of reliable clinical trial data.
Sponsors who embrace specialized manufacturing strategies are better positioned to meet the unique challenges of clinical trials, from managing complex supply chains to delivering innovative new medicines. By carefully selecting the right manufacturing approach, organizations can maximize the benefits of their clinical trial materials and drive successful outcomes for both patients and the pharmaceutical industry.
Collaboration and Cost-Effectiveness in Modern Clinical Manufacturing
With the increasing complexity of drug development, cost-effective planning and expert collaboration have never been more important. Many organizations partner with a seasoned manufacturing organization or CDMO to provide guidance on GMP requirements, scaling up for larger scale production in phase II or phase III clinical studies, and solving unique bottlenecks in the clinical manufacturing process. Integrating quality control, flexible production solutions, and clear lines of communication enables companies to adapt to new treatments, unforeseen challenges, and urgent regulatory demands. Ultimately, combining internal know-how with external expertise enhances the likelihood of success while controlling costs and maximizing speed to clinical milestones.
Mastering every aspect of CTM manufacturing is indispensable in today’s pharmaceutical landscape. At our specialized facility in Jura, Switzerland, we are experts both in clinical and commercial manufacturing. We combine advanced technology, strict cGMP compliance, and deep experience to support your projects with the highest quality and reliability—helping you bring innovative therapies to patients safely and efficiently.
Frequently Asked Questions (FAQ) About Clinical Trial Material
What is clinical research material?
Clinical research material includes all drug products, comparators, and placebos produced under strict guidelines expressly for safe and effective use in clinical trials.
What is a clinical material?
Clinical material is any substance—such as a drug, placebo, or control—made specifically for administration to human subjects within clinical studies under robust regulatory oversight.
What is trial material?
Trial material consists of investigational medicinal products, placebos, and comparators that have been manufactured, packaged, and documented to comply with regulatory standards for use in clinical trials.
What is the substance given in clinical trials?
This is most commonly the investigational drug or investigational medicinal product (IMP), occasionally paired with a placebo or comparator, administered to patients to test safety, quality, and efficacy as required by the trial’s design.